A total of 10 new interactive case studies have been added to our electronic fetal heart monitoring (eFM) programme – enabling healthcare professionals to test their cardiotocograph (CTG) skills in a virtual ward setting.
The award-winning eFM programme, which is suitable for both midwives and obstetricians, covers all aspects of intrapartum electronic fetal monitoring.
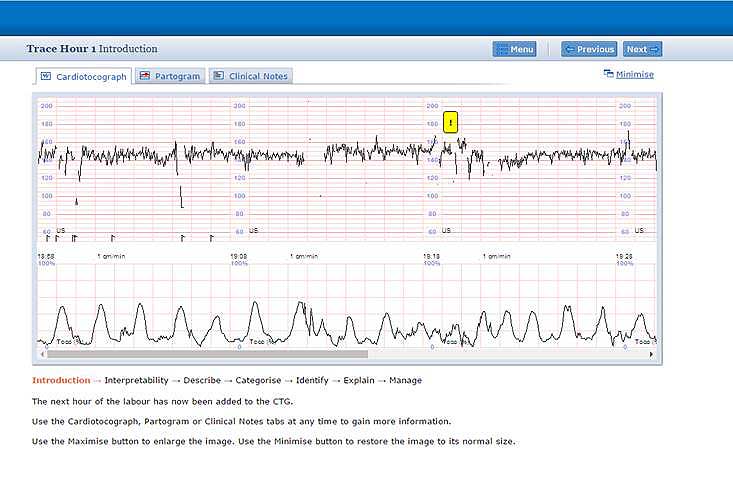
The case studies, which include clinical details and heart traces from real-life labours, reflect the latest care guidelines from the UK’s National Institute for Health and Care Excellence (NICE).
Jimi Jibodu, Clinical Lead for the programme, said: “You can look at the clinical information, make a judgement and decide on an appropriate management plan. This provides invaluable experience that is not currently available elsewhere.”
Using clinical details from real-life labours
Learners can work through each case study and look at:
- whether there are any risk factors for intrapartum fetal hypoxia
- classifying and defining the EFM
- distinguishing between ‘normal’ and ‘abnormal’ traces
- explaining the reasons for the FHR appearance
- choosing appropriate management options.
Using the new case studies, learners are also asked to recognise the types of decelerations, understand the different types of hypoxia and anticipate CTG changes that may occur if hypoxia develops.
Each case study takes around 30 to 45 minutes to complete. Learners can compare their performance with that of leading clinical experts.
The programme includes a mix of learning and test case studies. The test cases are scored and carry CPD points while the learning case studies are designed more for reflective learning. The learning cases are particularly useful in a group study setting – enabling users to pause the trace and discuss any specific aspect.
Alongside the case studies, eFM also includes knowledge sessions, self-assessment questions and a comprehensive e-library. It is regularly updated to reflect the latest clinical guidance. Further case studies will be added later this year.
eFM has been developed in the UK by the Royal College of Obstetricians and Gynaecologists, the Royal College of Midwives and NHS England e-Learning for Healthcare.
For further information, go to the eFM e-learning programme page.




